Morgan Dixon is the Head of Community at Swehl, a digital platform that provides streamlined tools, inclusive education, and safe spaces for parents to connect.
It still feels like it was yesterday. I was hysterically crying in the middle of the departures terminal of Newark Airport, suitcase wide open, everyone in the vicinity staring at me. It was the final day of my first trip away from my 16-month-old son, and I was desperate to get on the plane home to L.A. But, my suitcase had a battery pack and needed to be unscrewed before boarding. How on Earth would I get a screwdriver in the middle of an airport terminal?
By this point, the flight had been missed. My poor Uber driver, who dealt with my compulsive demands to take bizarre routes while I was sweating and crying, constantly tried to calm me down, assuring me I could find another flight. After arriving at the airport, the kind woman at the United desk could sense my unsettled energy and booked me on another flight that was leaving soon. I momentarily felt a sense of relief; I’d be able to see my baby tonight.
I ran as fast as I could to security, exhaling loudly as I waited to get through a line that seemed to have not moved in 20 minutes. I arrived at my gate, went to board, and, almost as in slow motion, the gate agent told me I couldn’t board the plane unless I removed said battery pack. I immediately started to feel hot and dizzy. I started crying and was acting confused. People gathered around, primarily as voyeurs, a few who felt for me and wanted to help. A man and his son flagged down a maintenance worker and tried to find a tool to get the battery pack out (to no avail).
It was 9 P.M., and the shops were all closed, or else I would have purchased a new bag. I would have given someone thousands of dollars if they could have offered me a solution. Eventually, an older woman emptied her tourism gift shop bags and handed them to me so I could shove in my belongings and carry them on. My suitcase was splayed open on the ground, underwear and all exposed. But what was most exposed at that moment to everyone but me were the depths of my postpartum anxiety.
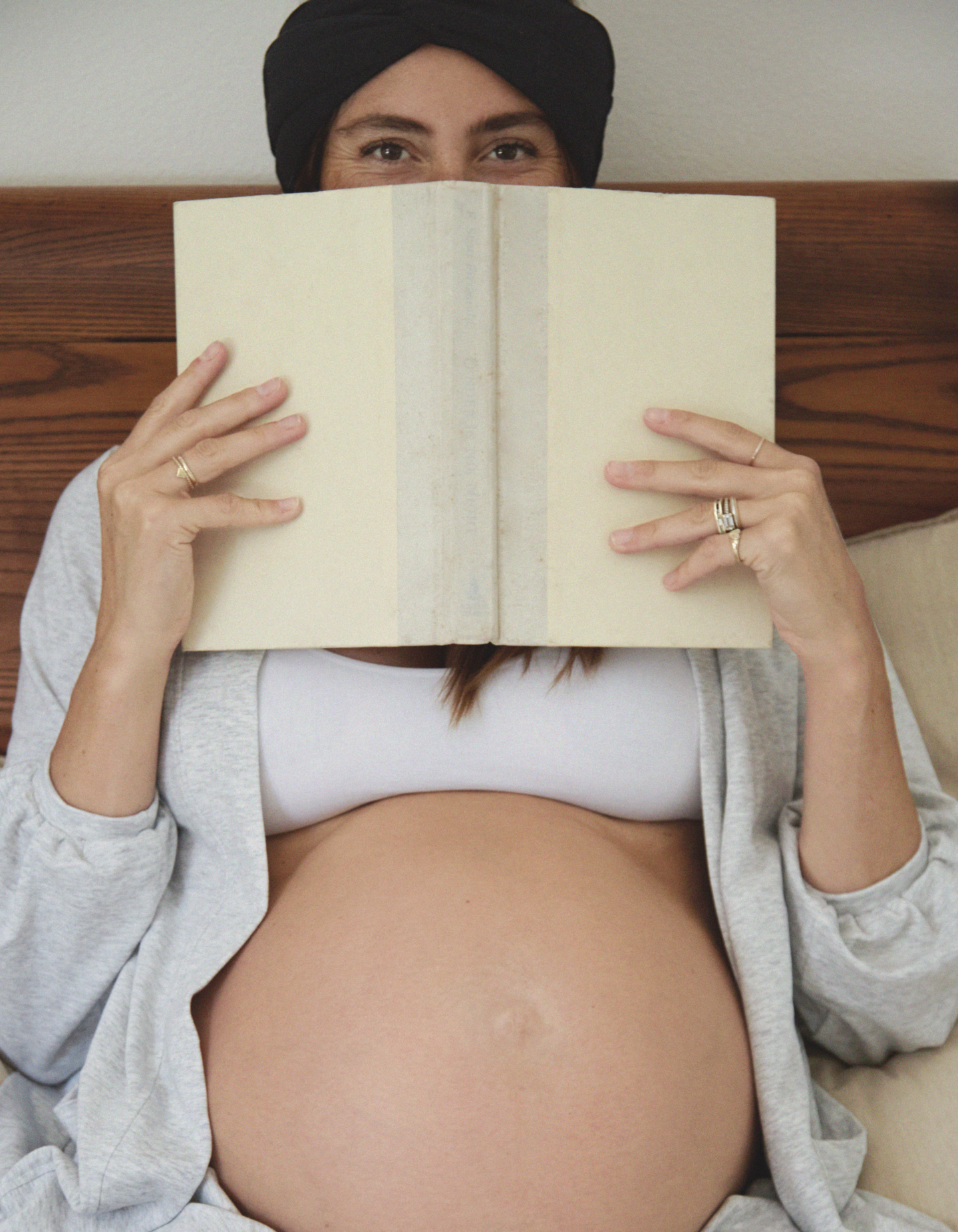
To be frank, before getting pregnant, I hadn’t heard many great things about motherhood. Yes, people loved their babies, but what followed that sentiment always seemed very conflicting, almost as if they were all yearning for the life they had before welcoming the baby and desperate to find the person they were before becoming “mom.” Stories of women hating their partners, lamenting that their bodies were never the same—they were all exhausted. I also wasn’t someone who felt connected to my baby during pregnancy, which left me feeling unsettled, to say the least. All in all, I had no idea what I was in store for, but I did know that I was apprehensive about what life would look like in the near future.
I went into labor two weeks early, and nine hours later, in the greatest moment of my life, I met my baby boy, Gray. Labor was, dare I say, fun? I only had to push a few times, and I was so into the whole process I reached down and pulled him out on my own. Later, I cut the umbilical cord myself. My son latched on to my breast about 10 minutes after giving birth, and we never had any breastfeeding issues. I was in a constant state of euphoria and finally felt like I’d found my purpose in life. All of these terrifying anecdotes I’d heard? None of them applied to me.
Sleep was something that literally everyone had told me would be hard to come by, but at 12 weeks old, Gray was sleeping from 8 pm-7 am; this baby was an actual dream! I had started a new mom’s group a few weeks earlier, and the woman who ran it mentioned that she was hospitalized for a few days after having her baby, so she had to pump to maintain her supply and for the baby to have bottles while recovering. I remember thinking—in my mind, a very rational thought—that I should start pumping to create a supply in case I was ever hospitalized. So, as my baby slept for eleven-hour chunks of time, I would wake up 3-4 times a night, sometimes more, to pump for 20 minutes. He would breastfeed several times a day, but I’d also pump once or twice, or more, throughout that.
I wasn’t heading back to a full-time job, so pumping this frequently was not necessarily out of necessity. I eventually had to purchase a deep freezer to store all the milk. Thinking about this possible future hospitalization also made me acutely aware of my health and possible mortality. I had a baby to care for now. I was his mother, and he needed me—what would happen if I got sick? Like, really sick?
That’s when I started to Google random symptoms I’d be feeling. From fatigue to a headache to dehydration, I’d find an article that linked almost anything to a terrifying and life-threatening illness. It got to a point where the hypochondria was so bad that even walking into a doctor’s office, I would feel faint out of fear of what they were about to tell me—eventually, feeling faint turned into actually fainting. Out loud, I would justify that it was because ‘I hadn’t eaten enough’ or that ‘I am a fainter, it’s no big deal.’ Objectively, I knew that my actual reasoning sounded crazy, yet I still felt wholly validated and rational in my mind.
Related: I’m SUPER Anxious About Having Sex for the First Time Postpartum
Next began the obsessive fears that something would happen to my baby. While on walks, I would avoid walking under trees if a branch fell and landed on his stroller. I’d make sure he was out of the kitchen whenever I had to use a knife in case I tripped while holding it, and it flew out of my hands and toward him. I loved this child so much—the world just started to seem like an increasingly scarier place. Around his first birthday, he weaned from breastfeeding, and I stopped being able to sleep. I was wired all night and would lie there obsessing over the fact that I wasn’t sleeping. I feared that it would make me a bad mom because I wouldn’t be able to be as present or energetic as I wanted to be. Exercising always energized me no matter how tired I felt, and I found a specific class that I loved, but the stress of getting back home from the studio was almost debilitating. I remember running out of class, jumping in my car, and frantically driving home to return to my baby. Each time, I found him there, completely content and happy. We had a lovely nanny who adored him and made him feel incredibly loved and secure in my absence. However, I would obsessively loop the same thought over and over for the next several hours: that I was a bad mom for leaving him and that everyone knew it.
The next several months got progressively worse. My obsessive thoughts started infiltrating my life, and my health fears and safety concerns became crippling. Here is the craziest part: no one would have ever known anything was wrong. I genuinely adored motherhood and adored my baby even more and felt undeniably bonded with him. Despite everything I’ve mentioned, I was simultaneously delighted. No part of me wanted to go back to a life before parenthood. I had lots of mom friends, was very social, and in so many ways, was loving this phase of life. But that’s the thing about postpartum anxiety. It isn’t obvious, and it’s very difficult to recognize symptoms in yourself as they arise. So often, we hear about postpartum depression and the telltale signs of feeling disconnected from your baby and motherhood, like hopelessness, anger, and a general loss of interest. I never felt any of these things; I felt the exact opposite.
I genuinely believed that my behaviors were making me a “better” mom, albeit hyper-vigilant. Pumping a lot? Great for my baby! Taking extra safety precautions? Again, a good thing! Occasionally, I caught an eye roll or underhanded comment from my partner or family about my hypochondria, but no one ever said, “Morgan, I notice that you are starting to have some obsessive thoughts and behaviors. How are you doing with everything?”
That trip to New York was the straw that broke the camel’s back. Even before the airport fiasco, I was in a full-fledged fight or flight. I didn’t want to go on this trip, but my partner (and society) convinced me it was important to do something like this for myself. From the second we left L.A., I wanted time to speed up. I felt like I was missing a limb. I just wanted to get it all over with so I could say I did it and then return home to my child. I felt utterly disconnected from my body the entire trip. I remember looking in the mirror and not even recognizing myself. I love New York, having worked there for years, and the city’s energy always recharged me—but not this time. Things were loud and made me anxious. I hated the chaos and just wanted to sit in the hotel room.
When I finally made it home to L.A., I acknowledged that while I had some stressful things happen while trying to get back to L.A., my reaction was not “normal.” I knew I had to get help. A year prior, as a preventative measure, the facilitator of the mom group I had joined shared a list of mental health professionals specializing in postpartum care. Ironically, the place that caused my first obsessive thought cycle was also the resource that provided me with the help I needed. I found an amazing psychiatrist who was warm and caring and a mother herself. About six minutes into explaining what I had been going through, she shared that my experience was quite common: it was called Postpartum Anxiety, and I specifically was dealing with intrusive thoughts and OCD. She reassured me that I was still a great mother and that there was a way for me to feel better. I still have trouble articulating the relief that washed over me.
Related: Maternal Mental Health Apps Worth Downloading
I was prescribed an SSRI, which helped almost immediately, along with some cognitive behavioral therapy. I was also referred to an acupuncturist to help balance my hormones. Studies have shown that hormones contribute heavily to postpartum mood disorders, which tracks with the timing of my worsening symptoms. Things escalated for the worse as I weaned my son from breastfeeding, which can cause significant hormonal dysregulation, and for me, it had a lot to do with dopamine imbalance (which can specifically cause intrusive thought OCD). Within a few months of treatment, I felt like a different person. The therapy helped immensely with controlling my thoughts, and I stopped taking my medication fairly quickly. I could finally experience motherhood without being a prisoner to my obsessive thoughts.
Postpartum anxiety affects nearly 35% of new moms (although that number is likely much larger) and can present itself much later in the journey, as it did with me. When it comes to postpartum care, most women get the generic questionnaire at their OB/GYN’s office six weeks after giving birth, and beyond that, support quickly dissipates. Despite what we’d like to believe, mothers face judgment every step of the way. As such, they commonly struggle in isolation for far too long before seeking help.
Even as I write this all out, I am nervous about what people will think of me if they find out I struggled. Will they think I was a bad mom? Will they think that I’m complaining and being too self-indulgent? I have a beautiful life and a sound support system. Will they think I’m crazy? I was fortunate to have access to the best resources—imagine the massive population of mothers drowning in their shame without any options.
Through my experience, I learned that two contrasting things can simultaneously be true. I loved motherhood and my child more than I ever could have imagined, and I was struggling. That duality is present throughout motherhood, and we’re often just expected to figure that out ourselves. We’re told to adjust to our new lives, navigate the return to work mere months after giving birth, and manage our health and well-being while maintaining our friendships, being good partners, and keeping a tiny human alive. We are faced with an impossible task, yet society still collectively gasps when presented with statistics detailing that postpartum mental health issues are continuously rising.
There’s no question that we need to normalize not being okay.
Mothers deserve to be presented with a new narrative supporting openly discussing the duality, expectation, and struggle. Experiencing postpartum depression, anxiety, or even questions over your purpose and identity in no way labels you a bad parent. On the contrary, being brave enough to seek help makes you an even better parent who is already modeling to your child that you prioritize your well-being. In the end, I am grateful for my journey with postpartum anxiety. I became more enlightened about my body, learned how my hormones affect me, and acquired tools and coping mechanisms should I ever have another bout with postpartum anxiety. Equally, my experience led me towards a new career, fueled by a new curiosity about the physiology of new motherhood.
I openly share my story now because I have encountered many women who have felt relief when hearing it. If I can help even one mom feel less alone, then my vulnerability is worth it, scary as it sometimes is. The first step to normalizing this widespread experience is to start sharing our stories in hopes that our generation’s collective power can ensure that future mothers have the support that has been lacking for us.